One question that is often asked is ‘When should an orthotic be used in conjunction with the patients treatment program?
Many practitioners grapple with this issue and it can be confusing, especially if orthotic therapy is not used regularly in clinical practice.
One starting point is to examine the common conditions where orthotics are or have been recorded as being effective. The use of orthotics can be beneficial in many circumstances and so practitioners should be aware of the application and treatment. Doing this will make available to their patients treatment choices when attending to lower limb biomechanical conditions.
Practitioners should use their own modality in conjunction with orthotic therapy, or develop relationships with practitioners from other modalities, thus combining treatments to provide the patient with a holistic regime.
Orthotic therapy is not a definitive treat-ment, it should be regarded as just one part of the treatment protocol.

The common conditions that an orthotic can treat include:
Bunions
usually caused by a short 1st metatarsal1 and aggravated by excessive pronation at mid-stance to toe off 2.
Ball of Foot Pain
collapsing and rotating of the metatarsals result-ing from excessive pronation.
Plantar Fasciitis / Heel Spur
excessive pronation causes the fascia to elongate and tear from the calcaneal attachment. Spurs are a secondary compensation.
Severs Disease
(children’s heel pain) – related to excessive pronation and growth spurts in children and affects sporting children more than sedentary ones.
Achilles Pain
excessive pronation and supination creates a point of pain stress point.
Shin Splints
lateral, medial, anterior – excessive pronation and supination are key contributing factors.
Knee Pain
collateral ligament strain due to excessive pronation and supination factors.
Osgood Schlatters Syndrome
occurs due to a combination of tibial tuberosity immaturity and quadriceps tightness3, growth spurts and tibial rotation factors.
Hip Pain
due to structural or functional leg length and supination factors including tight external hip rotators.
Low Back Pain
Unilateral and bilateral pronation, and structural and functional leg length causing stress on the lower back L1-L5.
Leg Length Syndrome
when a structural leg length difference is evident the long leg may excessively pronate as compensation to level the pelvis.
A report by The American College of FOOT & ANKLE ORTHOPEDICS & MEDICINE entitled Prescription Custom Foot Orthoses – Practice Guidelines, December, 2006 names the following conditions as being treatable with orthotic therapy :
1. Proximal Lower Extremity Pathology A. Shin Splints B. Tendonitis (Tenosynovitis) C. Posterior Tibial Dysfunction D. Chondromalacia Patella (Runner’s Knee, Patellofemoral Syn-drome) E. Iliotibial Band Syndrome F. Limb Length Discrepancy
2. Arthritides A. Inflammatory Arthri-tis, B. Rheumatoid Arthritis, Psoriatic C. Arthritis, Other Inflamatory Ar-thritides D. Osteoarthritis
3. Mechanically Induced Pain and Deformities A. Pes Cavus, Haglund’s Deformity B. Hammer Digit Syndrome C. Functional Hallux Limitus, Hallux Limitus and Hallux Rigidus D. Plantar Fasciitis E. Equinus F. Sinus Tarsi Syn-drome G. Tailor’s Bunion (Bunionette) H. Hallux Abducto-Valgus (Hallux Val-gus, Bunion) I. Pes Planus J. Metatarsal-gia K. Sesamoiditis L. Morton’s Neuroma (Intermetatarsal Neuroma)
4. Pediatric Conditions A. Calcaneal Apophysitis B. Genu Varum and Genu Valgum C. Tarsal Coalition D. Metatarsus Adductus 5 . Sensory Neuropathies A. Peripheral Neuropathy B. Charcot Neuroarthropathy (Charcot Foot)C. Tarsal Tunnel Syndrome So what is the starting point? And when should I use orthotics? First ,establish if the patient presents with a condition that is recorded as, being able to be treated with orthotics.
Check for pronation or supination. If the patient pronates, this will often be an underlying factor to many of the conditions mentioned above, treatment with orthotics to realign and control the rearfoot and support the longitudinal arch should be undertaken.
Identifying Lower limb biomechanical anomalies and foot mechanics issues relating to both pronation and supination will be a key treatment to realigning and controlling the rearfoot with orthotics.
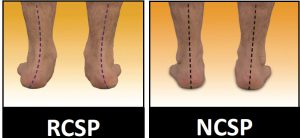
Identify the amount of excessive pronation or excessive supination by correcting the foot to neutral and then allowing the patient to rest and relax their feet (NCSP and RCSP)* this will allow you to identify whether the patient will require a corrective orthotic product.
Next, check structural leg length and if a heel lift is required attach to the orthotic for the short leg, start by using ½ the measured amount or a 4mm heel lift addition. The long leg may be excessively pronating as compensation and will need to be supported by the orthotic. Never use a single orthotic, always prescribe a pair as this will maintain correct foundational balance.
If the foot is supinating the patient will experience jarring in the foot and to the upper structure, and will often have a rigid high arched foot type. This type of foot commonly exhibits a forefoot valgus deformity. The pes cavus type foot is not that common – about 8 – 9% of the population may present with it.
In this case an orthotic is required to control the supination by maintaining the Ideal / Neutral Calcaneal Stance Position(NCSP), use a forefoot addition to treat the forefoot valgus, whilst providing the patient with comfortable support.
Prescribing an orthotic for your patient base is easy as: 1, 2, 3
1. Identify the RCSP (patients Resting position).
2. Observe the NCSP (Neutral or corrected position) to identify the correct position for heat moulding the orthotic, and to help identify the pronation effect,
i.e. NCSP – RCSP = Total Pronation
Observation of Rearfoot positioning and Anterior positioning using ICB Anterior Alignment Method ( ICBAAM) see youtube.com/icbmedical
3. Check the leg length (manually) for any structural differences.
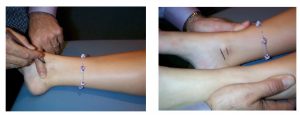
4. The Palpation for Supine Medial Malleoli Asymmetry Technique is an easy method which has been reported as having both Intra-examiner and inter-examiner reliability. The technique was clinically trialled at RMIT University 2005 by Gary Fryer4.
By following these simple steps more than 80% of the Lower Limb Biomechanical conditions practitioners see in the clinic on a daily basis can be treated effectively with orthotic therapy.
Patient’s should be instructed to wear their orthotics for 1-2 hours per day, increasing gradually over 1-2 weeks until it is comfortable wearing them full time. If discomfort is experienced, the patient should take the orthotics out of their shoes, and give their feet a rest. Continue until it is comfortable wear-ing the orthotics all day.
“When should orthotic additions be attached to the orthotic?”
Orthotic additions can be added on the subsequent consultation.
Forefoot & Rearfoot additions can be attached to the orthotics on subsequent visits – if required.
If you need any further assistance or advice with patient assessment, or prescribing orthotics View DLT Facebook, contact DLT Podiatry
email: sales@dltpodiatry.co.uk, or go to the website: www.dltpodiatry.co.uk