Orthotic therapy often is a therapy which involves some adjustment to the prescription of the treatment device. The therapy, rather than being a ‘one size fits all’ approach is one which requires working with the patient to get the desired result.
By that we mean that different conditions will require different treatment approaches and different orthotic prescriptions to meet patient expectations and to provide required results.
Orthotic devices are mechanical devices and often an alternative approach is required due to shoe styles and other issues which impede the treatment process.
One such issue is problematic movement of additions and in this instance the metatarsal dome placement on the orthotic device.
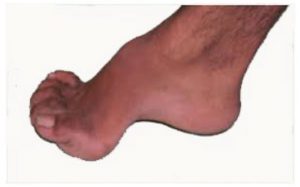
Issues that are most prevalent are:
1) Placement on the orthotic
2) Positioning of the dome in relationship to the patients foot.
3) Soft and firm domes which to use?
4) Movement of the dome.
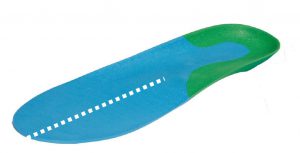
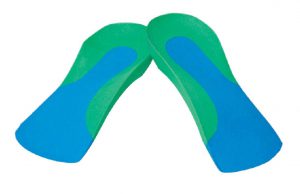
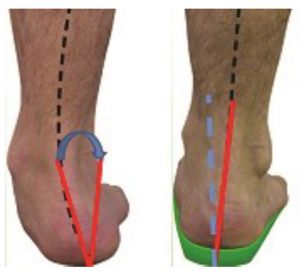
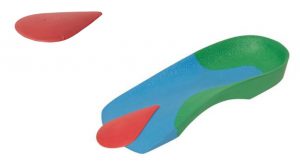
Usually ‘met’ domes are adhered to the dorsal surface of the orthotic.
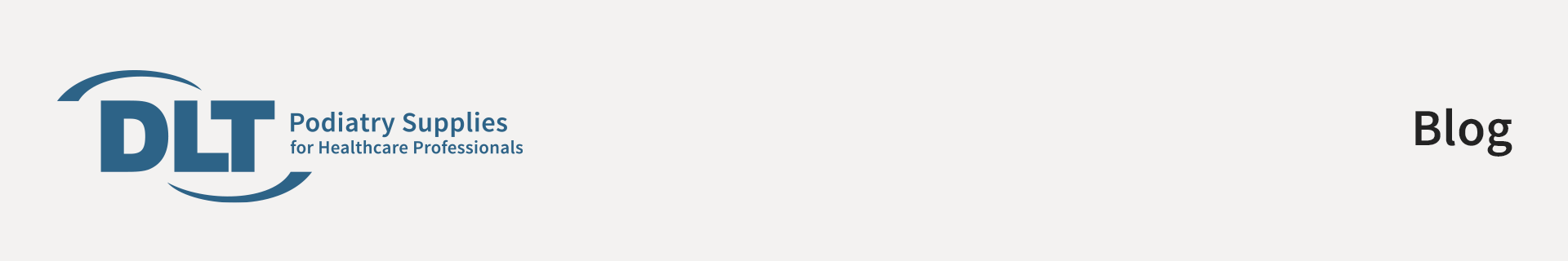
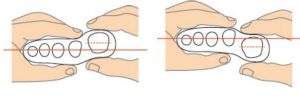
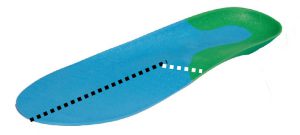
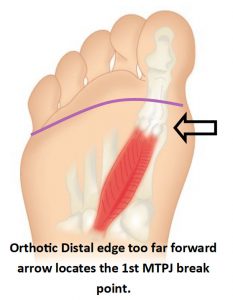
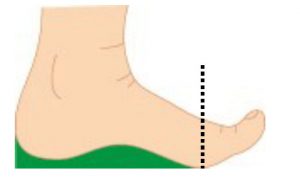
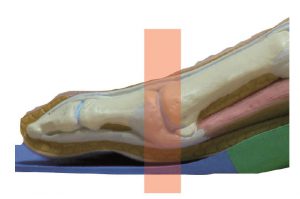
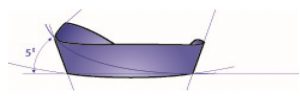
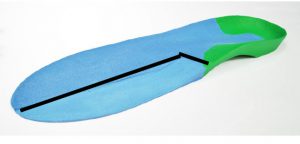
We advise that the distal edge of the dome should approximately 5mm forward to the distal edge of the orthotic device.
The positioning will lift the metatarsal shafts and not impinge on the metatarsal joints during toe off phase.
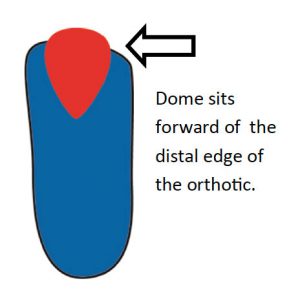
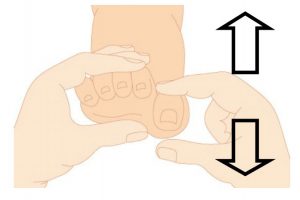
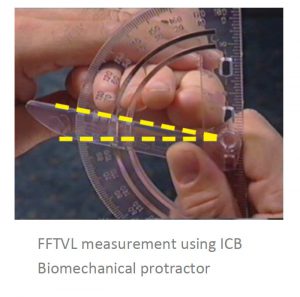
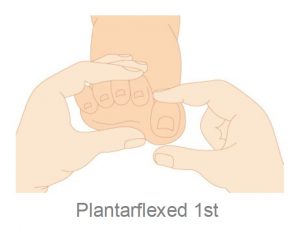
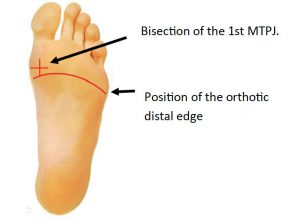
When using a Full length device practitioners will need to establish where the orthotic ‘distal’ edge sits on the orthotic device .
In this case just fold back the forefoot of the Full length to reveal the position of the bisection of the 1st MTPJ.
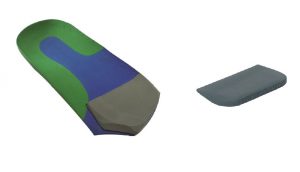
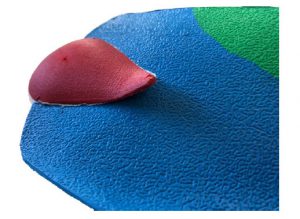
Soft as opposed to Firm domes can be a matter of preference, however, if correctly positioned the patient will not find the firm domes uncomfortable to wear.
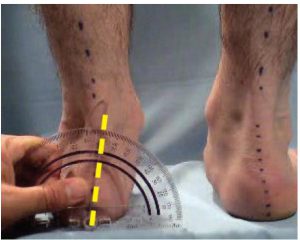
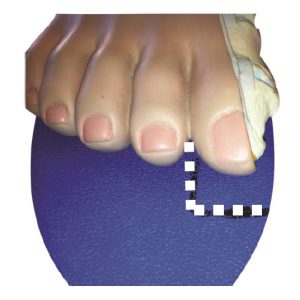
Positioning should be an outcome of the type of issues the patient present with, such as, pain or discomfort between 3rd & 4th or 2nd and 3rd met heads. Often a temporary placement is beneficial as the position can be adjusted until the patient feels that they are happy with the position. If the 3M tape is not sufficient to hold the dome in position then a more permanent fixing can be achieved with glue such as a spray glue.

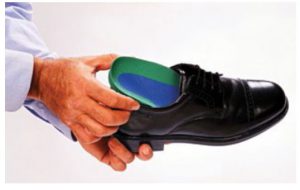
Often patients complain that the metatarsal dome addition has a tendency to peel off the dorsal surface due to getting caught on their socks as they place their foot into the shoe.
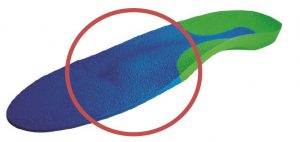
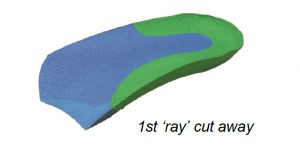
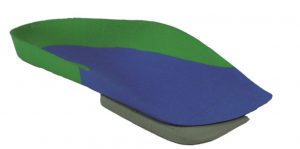
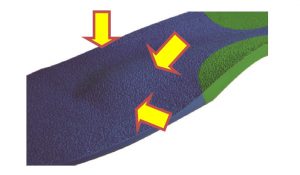
The remedy for this issue is to create an ‘intrinsic’ metatarsal dome, that is, create the metatarsal dome in the actual orthotic device– Intrinsic—built in or become part of the device.
Completing the intrinsic dome modification will remove the likelihood of the addition peeling off or getting caught on the patients sock.
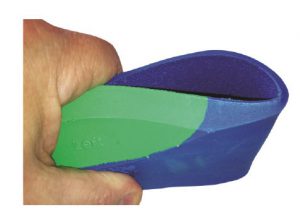
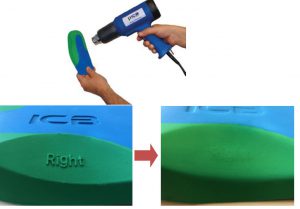
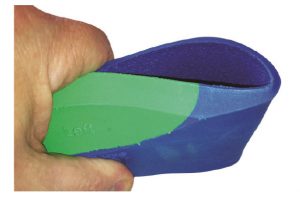
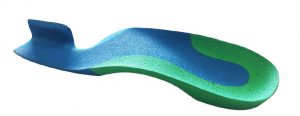
ICB orthotics are 100% EVA material which moulds well under heat and is highly adaptable. To effect this adjustment practitioners will need to establish the position on the patients foot where the metatarsal dome is to be positioned.
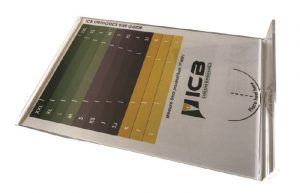
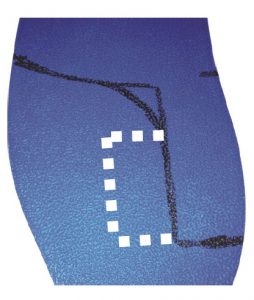
Place the correct size Dome—Small for small foot Large for Large foot on the Plantar surface of the orthotic and draw the shape of the dome.

Remove the Dome and using a Heat gun apply heat to area that you wish to deflect.
Next place the FIRM dome on a hard flat surface and position the orthotic on top in the correct position for moulding.
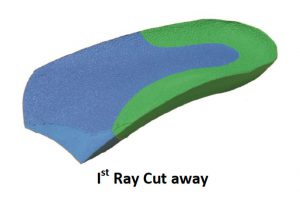
Once you are able to see the shape of the dome you can apply 3M tape to the dorsal surface of the dome in readiness to apply to the plantar surface of the orthotic.
At this point a decision can be made as to whether you wish to use the firm dome OR another material such as felt or poron to infill and maintain the shape of the in-built dome.
The shape can be cut and glued into the cavity and then ground flat on the base for the best fit.