A Dorsiflexed 1st Ray (Metatarsal) also known as metatarsus Primus describes a deformity in which the 1st Ray /Metatarsal lies in a dorsiflex position relative to the lesser metatarsals.
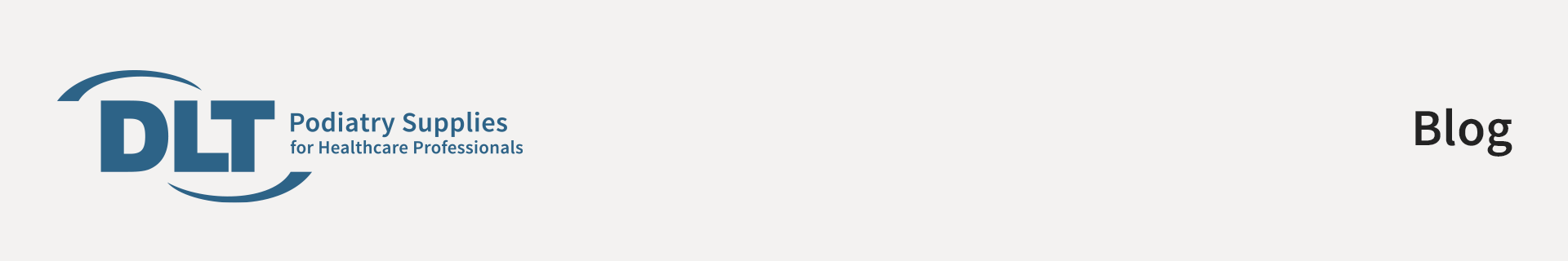
The first ray is made up from the first metatarsal and the medial cuneiform. The ray facilitates movement in all three planes however predominantly produces the frontal and sagittal plane movements of dorsiflexion coupled with inversion and plantarflexion with eversion. This is due to its axis being 45° to both of these planes.
The biomechanics of this condition and the compensatory mechanisms and the resultant limitations need to be considered to understand both the function issues and the possible treatment that will need to be proposed for this condition.
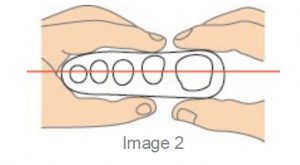
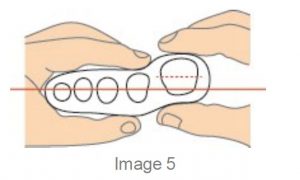
The first ray (metatarsal) normally sits parallel to the plane of the lesser rays with equal amounts of dorsiflexion and plantarflexion usually 5mm up and 5mm down to allow the required plantarflexion to enable 65° to 75 °of MPJ dorsiflexion during the propulsive phase.
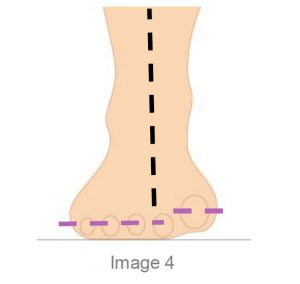
A Dorsiflexed 1st Ray is an osseus deformity where the lesser metatarsals sits lower to the bisection of the 1st Metatarsal when the foot is in the STJN position.
The condition may be congenital or acquired and is often referred to as ‘metatarsus primus elevatus’ or simply the prime metatarsal is elevated in reference to the lesser.
It should not be confused with Forefoot Supinatus as once the foot is placed in STJN the shaft can, with a supinatus, be plantarflexed. However, we should understand that the dorsiflexed 1st can be both fixed and or mobile in nature.
Because the 1st metatarsal is dorsiflexed it encourages the foot to collapse medially inhibiting the phalange from propelling over the 1st MTPJ, jamming occurs and a reduction in the ROM of the joint may be experienced.
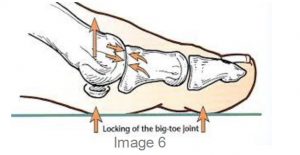
The result of this jamming will be a stiffening of the joint and often the patient will develop an adductory twist in gait to reduce the load on the 1stMTPJ, as this occurs callosity will develop on the medial aspect of the hallux.
The distal phalanx of the hallux can also be forced into dorsiflexion as a toe off compensation, causing a hole to wear on top of the shoe and thickening of the nail from the constant trauma on the dorsal toe.

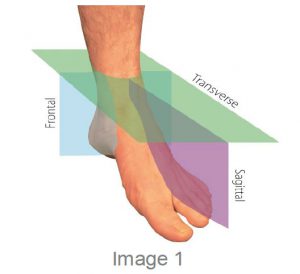
Clinical assessment of Metatarsal Phalangea Elevatus ( MPE) involves the evaluation of the sagittal plane position of the joint. The patient is evaluated in a non-weight bearing supine position with the subtalar joint in its neutral position (use the ICB AAM method) for Neutral.
As previously stated Metatarsus primus elevatus can be described as being congenital or acquired and can be further classified as a rigid, semi rigid, mobile or hypermobile deformity. A normal range of motion usually indicates a congenital deformity whilst an acquired.
MPE is characterised by an abnormal range of motion. This may be due to tibialis anterior contracture or associated with a forefoot supinatus.
The main issue is that the elevated metatarsal encour-ages the foot to function similar to a forefoot varus and excessive pronation is a key element as the foot collapses medially to allow normal ground contact in the toe off phase. Treatment will be a Morton’s ramp extension.
The purpose of the treatment is to allow a more normal ‘toe off’ to occur in the gait cycle by filling the gap under the 1st MTPJ whilst supporting the proximal hallux and thereby allowing earlier loading to occur.
To create the Mortons ramp to lift the proximal hallux this can be achieved by using a ICB 4° Forefoot addition (acts like a Morton’s ramp Image 9) to support the hallux and allow it to propel over the 1st metatarsal joint during toe off stage of gait.
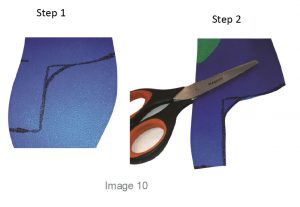
A Full Length orthotic can also be used to create a Morton’s extension, use the forefoot addition to provide the required lift. See image 10 add the addition and mould to the foot in Neutral. First mark out the Morton’s extension ramp shape , cut and use a hand grinder to smooth the distal edges.
Orthotic therapy is not an exact science, so be prepared to adjust the orthotic for the patient by adding or subtracting as needed.
General REFERENCES
1. Merriman, L.M. and Tollafield, D.R. (1995) Assessment of the Lower Limb. Churchill Livingstone, Singapore Figure 2: Evaluation of first ray position(Merriman and Tollafield, 1995)
2. Root M L, Orien W P, Weed J H., 1977 Normal and Abnormal Function of the Foot. Clinical Biomechanics Vol 2, Los Angeles
3.Merriman’s assessment of the Lower Limb 3rd Ed. Churchill Livingstone