Choosing the correct size orthotics for the patient can be somewhat of a minefield if practitioners do not follow the correct procedure.
SAVE 10% OFF ICB PRODUCTS WITH DISCOUNT CODE: 02ICB10 Offer online only!
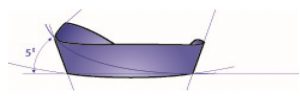
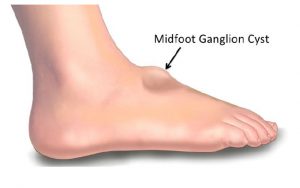
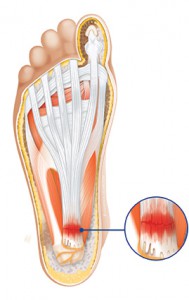
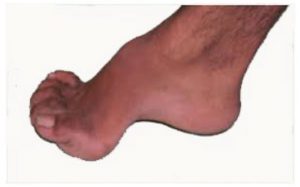
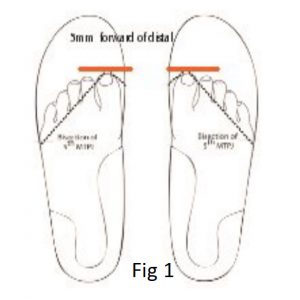
Orthotics in which the Distal edge of the orthotic (2/3 or 3/4 style) is too long can cause issues for the patient such as, Sesamoiditis.
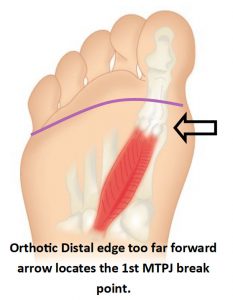
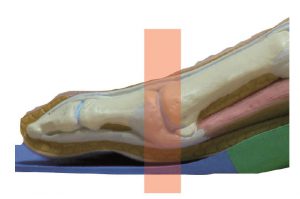
Sesamoiditis condition can occur when the 2/3 orthotic distal edge protrudes past the ‘break point’ of the foot and impinges the sesamoid apparatus.
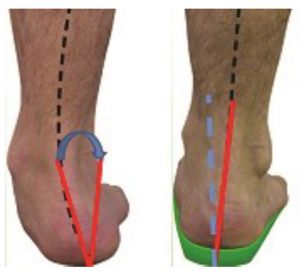
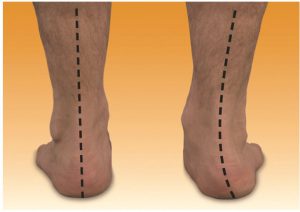
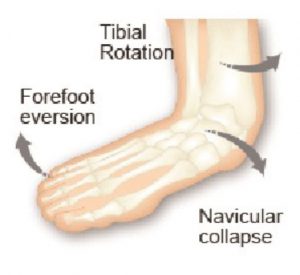
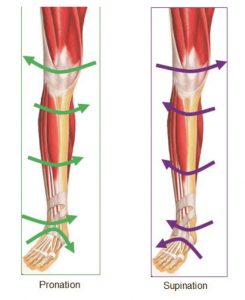
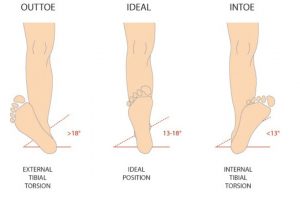
Orthotics that are too short can encourage the patient to excessively pronate due to the devices inability to maintain the longitudinal arch position. A further issue is excessive internal tibial rotation.
Therefore the simple act of prescribing the correct pre-made orthotic size can be either extremely beneficial or somewhat of an issue for the patient.
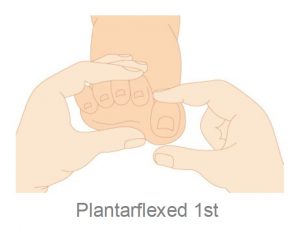
Usually the orthotic size is determined by the shoe size, however, often patients present with shoes that are 1 or 2 sizes larger than they really need based on reasons best known to the patient. In this instance the arch contour can be longer than the patient requires and the orthotic arch can impinge upon the patients 1st MTPJ causing irritation of the sesamoid apparatus.
If the product being used is able to be heat moulded well into the patients arch and attention given to the area beneath the 1st MTPJ to ensure that the arch does not impinge, then, a larger size to fit the shoe can be acceptable although this situation is not ideal. There are three ways to determine the correct size is:
1) use the patients shoe size
2) use the shoe sizing guide and
3) physical measurement of the device on the patient.
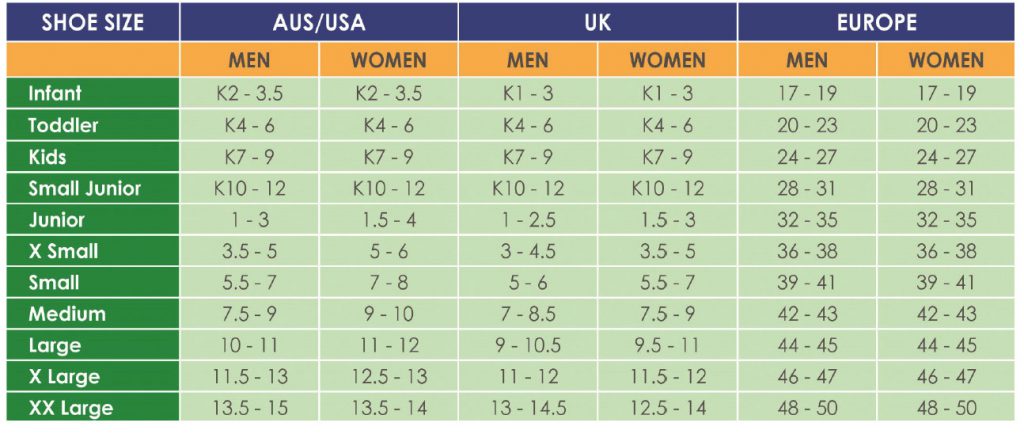
The issue with shoe sizing is that it appears that there is no standard shoe size guide worldwide and a size 8w may be a 7.5w or a 8.5 -9 w in another shoe brand and therefore physical measurement become the only reliable way to determine the correct size orthotic.
*Brooks * asics *New Balance
*Addidas *Nike *Misuna
*Saucony *Spenco All different sizing
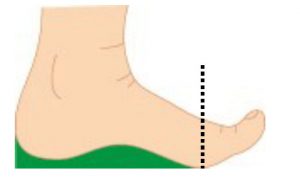
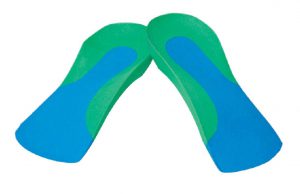
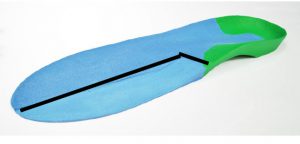
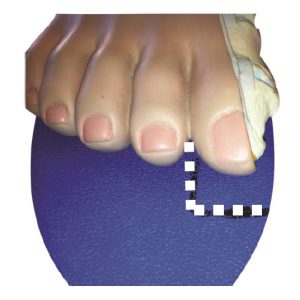
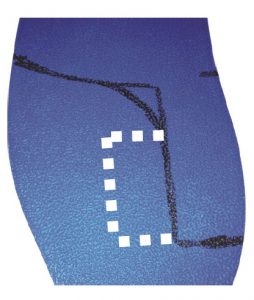
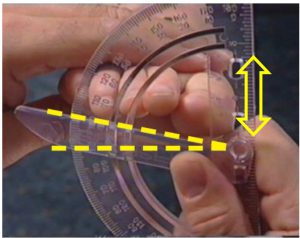
Placing the product on the base of the foot and observing the position of the orthotic distal edge will deter-mine the correct size. The Distal edge should be 5-10 mm proximal to the 1st MTPJ or ‘break point’ of the foot.
Full Length sizing fold back orthotic to identify the distal arch. position.
Note the position of the 1st MTPJ on the full Length product in the photo.
The joint should sit approx. 5-1 mm proximal to the joint to allow the foot to break at toe off stage of the gait cycle. Impingement of the joint is not recommended.
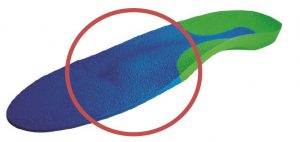
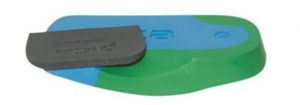
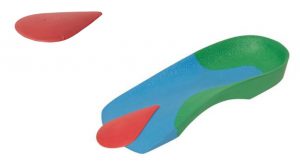
Some orthotic manufacturers provide sizing template guides (such as ICB below) however this is not a common practice.
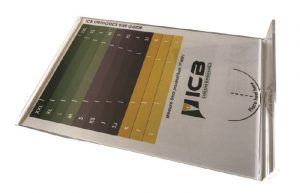
(Above : ICB sizing template)
Measurement on the foot is therefore considered as the most reliable way to measure the device for the patient.
Physical measuring is important when patients present with short arch or long arch , long and short toes.
Short arch may need to either choose a smaller size orthotic or heat mould the orthotic really well into the arch and concentrate the heat around and under the 1st MTPJ to contour the product and remove any pressure from the orthotic arch on the 1st MTPJ.
Long arch may require a larger size orthotic and then the length will need to be trimmed to fit the shoe.
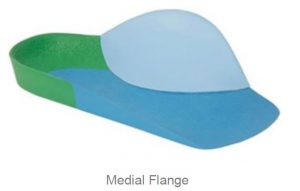
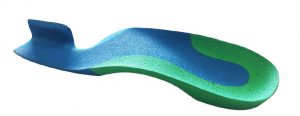
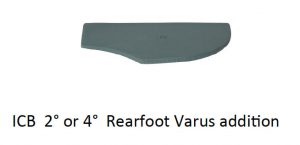
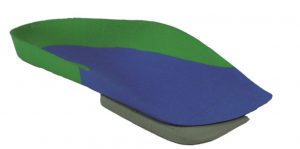
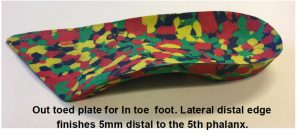
Wide feet can be problematic as the general orthotic designs in the marketplace do not cater for wide feet and practitioners may have to choose a product such as the ICB DRESS 2/3 Style design which has a lateral skive to allow for the foot to splay laterally.
Shorter wide feet can be adequately catered for with this product as the distal edge can be trimmed to reduce the length of the orthotic design
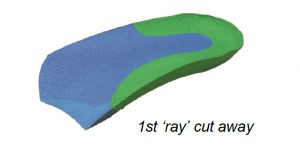
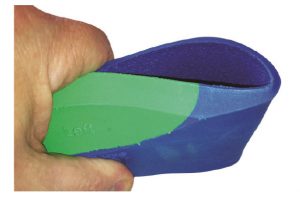
(above ICB Dress style with lateral edge removed to allow for patients with wide feet.